Psychiatric Follow Up Note Template
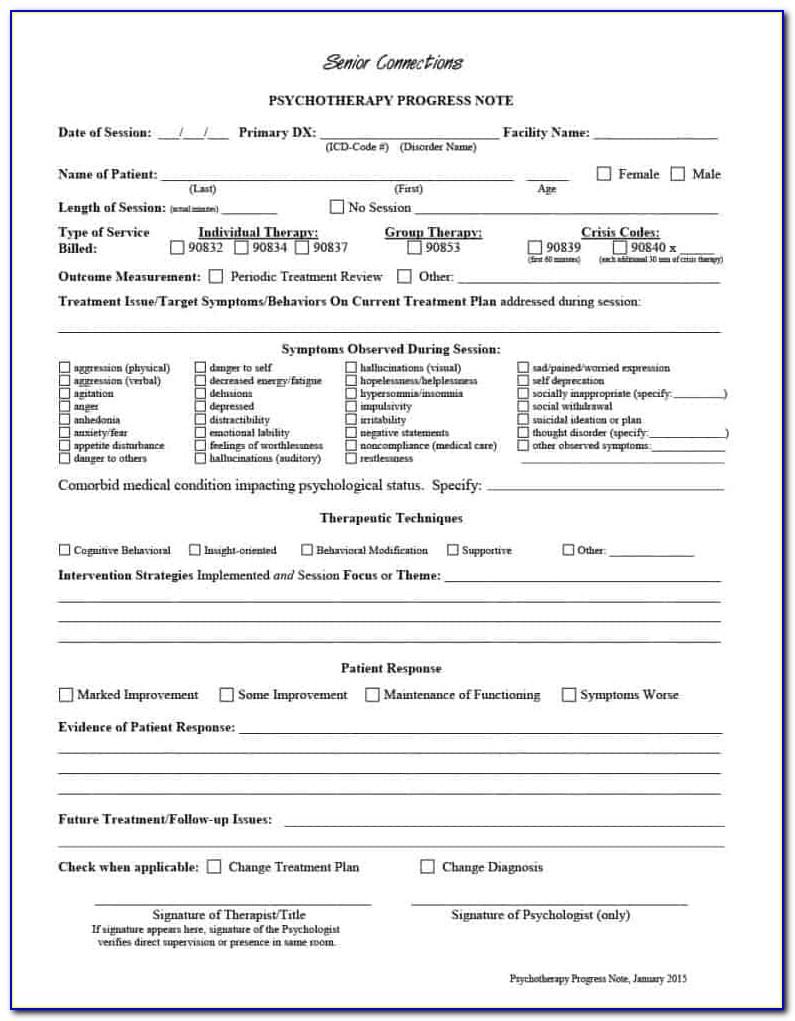
Psychiatric Follow Up Note Template - This post is long overdue and caution, it is long. May 19, 2022 psych team. Family history of suicide is noted. Pertinent system irritability mood instability heightened anxiety attention problems troubled by hallucinations. Web [select name=variable_2 value=in the past 24 hours|in the past 48 hours|since admission], patient [select name=variable_3 value=has|has not] required. Biopsychosocial assessment mental status exam couples therapy notes. Web of the evaluation may or may not lead to a specific psychiatric diagnosis. Use this outpatient psychiatric progress note to gather. 1) general psychiatric evaluation, 2). Web attention and organization were good up until this past week (associated hpi scoring: Web download now of 2 psychiatry follow up s: This post is long overdue and caution, it is long. Web [select name=variable_2 value=in the past 24 hours|in the past 48 hours|since admission], patient [select name=variable_3 value=has|has not] required. Web outpatient/office psychiatric progress note counseling and/or coordination of care (99214 or 99215) patient’s name: 6 elements = extended pfsh stopped attending. 6 elements = extended pfsh stopped attending school; 1) general psychiatric evaluation, 2). There are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan). Web of the evaluation may or may not lead to a specific psychiatric diagnosis. Web [select name=variable_2 value=in the past 24 hours|in the past 48 hours|since admission], patient [select name=variable_3 value=has|has. Web ccc bhp follow up appointment note template o date: Biopsychosocial assessment mental status exam couples therapy notes. Web this will also give you a good understanding of the clinical content available in our notes templates. 1) general psychiatric evaluation, 2). No guilt / grandiose / somatic delusions. Pertinent system irritability mood instability heightened anxiety attention problems troubled by hallucinations. There are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan). Family history of suicide is noted. Ad progress note & more fillable forms, register and subscribe now! This post is long overdue and caution, it is long. There are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan). No guilt / grandiose / somatic delusions. Biopsychosocial assessment mental status exam couples therapy notes. O individual o family o conjoint (e.g., with. X, a 56 yowf with a history of paranoid schizophrenia and major depressive disorder, presents to the clinic for f/u. Web outpatient/office psychiatric progress note counseling and/or coordination of care (99214 or 99215) patient’s name: Ad progress note & more fillable forms, register and subscribe now! Web ccc bhp follow up appointment note template o date: Web the patient identifies the following symptoms: Web this will also give you a good understanding of the clinical content available in our notes. Web download now of 2 psychiatry follow up s: There are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan). Web outpatient/office psychiatric progress note counseling and/or coordination of care (99214 or 99215) patient’s name: Web the patient identifies the following symptoms: 6 elements = extended pfsh stopped attending school; Web with our free online outpatient psychiatric progress note template, you can instantly generate a new note — then sync it to your other accounts from 100+ popular apps,. Ad progress note & more fillable forms, register and subscribe now! X, a 56 yowf with a history of paranoid schizophrenia and major depressive disorder, presents to the clinic for f/u.. Web [select name=variable_2 value=in the past 24 hours|in the past 48 hours|since admission], patient [select name=variable_3 value=has|has not] required. Pertinent system irritability mood instability heightened anxiety attention problems troubled by hallucinations. Web attention and organization were good up until this past week (associated hpi scoring: Web with our free online outpatient psychiatric progress note template, you can instantly generate a. X, a 56 yowf with a history of paranoid schizophrenia and major depressive disorder, presents to the clinic for f/u. Web [select name=variable_2 value=in the past 24 hours|in the past 48 hours|since admission], patient [select name=variable_3 value=has|has not] required. Use this outpatient psychiatric progress note to gather. Three types of clinical psychiatric evaluations are discussed: O 15 minutes o 30. May 19, 2022 psych team. Web the patient identifies the following symptoms: Ad progress note & more fillable forms, register and subscribe now! O 15 minutes o 30 minutes o 45 minutes o 60 minutes o type: Web with our free online outpatient psychiatric progress note template, you can instantly generate a new note — then sync it to your other accounts from 100+ popular apps,. There are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan). 1) general psychiatric evaluation, 2). Web outpatient/office psychiatric progress note counseling and/or coordination of care (99214 or 99215) patient’s name: Web [select name=variable_2 value=in the past 24 hours|in the past 48 hours|since admission], patient [select name=variable_3 value=has|has not] required. Pertinent system irritability mood instability heightened anxiety attention problems troubled by hallucinations. Three types of clinical psychiatric evaluations are discussed: Web of the evaluation may or may not lead to a specific psychiatric diagnosis. No guilt / grandiose / somatic delusions. 6 elements = extended pfsh stopped attending school; Use this outpatient psychiatric progress note to gather. X, a 56 yowf with a history of paranoid schizophrenia and major depressive disorder, presents to the clinic for f/u. Biopsychosocial assessment mental status exam couples therapy notes. This post is long overdue and caution, it is long. O individual o family o conjoint (e.g., with. Web this will also give you a good understanding of the clinical content available in our notes templates. O individual o family o conjoint (e.g., with. There are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan). Family history of suicide is noted. Ad progress note & more fillable forms, register and subscribe now! Biopsychosocial assessment mental status exam couples therapy notes. Web attention and organization were good up until this past week (associated hpi scoring: Pertinent system irritability mood instability heightened anxiety attention problems troubled by hallucinations. No guilt / grandiose / somatic delusions. Web with our free online outpatient psychiatric progress note template, you can instantly generate a new note — then sync it to your other accounts from 100+ popular apps,. X, a 56 yowf with a history of paranoid schizophrenia and major depressive disorder, presents to the clinic for f/u. May 19, 2022 psych team. This post is long overdue and caution, it is long. Web outpatient/office psychiatric progress note counseling and/or coordination of care (99214 or 99215) patient’s name: Web the patient identifies the following symptoms: O 15 minutes o 30 minutes o 45 minutes o 60 minutes o type: 1) general psychiatric evaluation, 2).History Of Present Illness Example Psychiatry Global History Blog
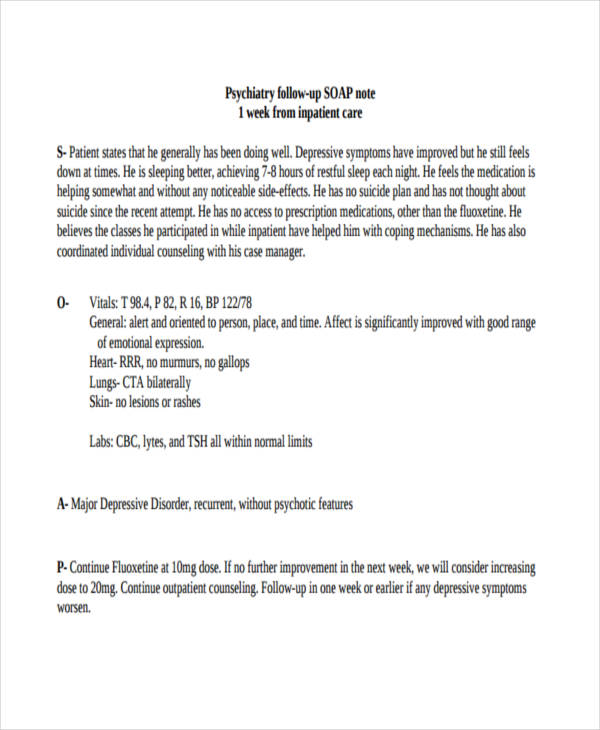
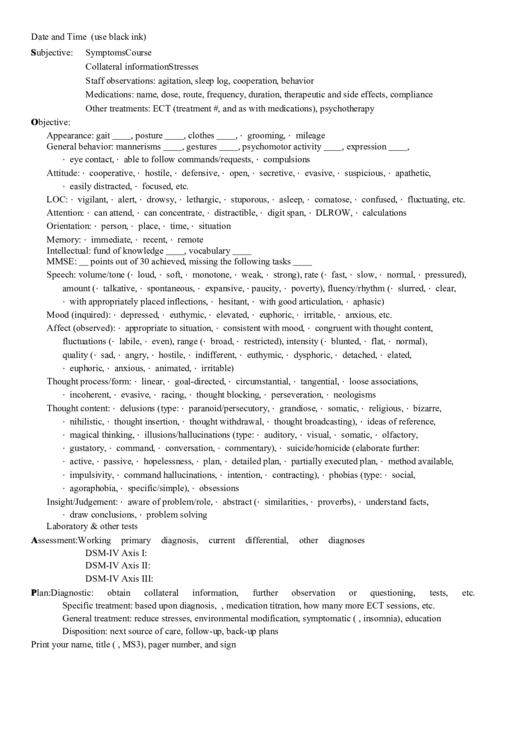
SOAP Note Examples 19+ in PDF Examples
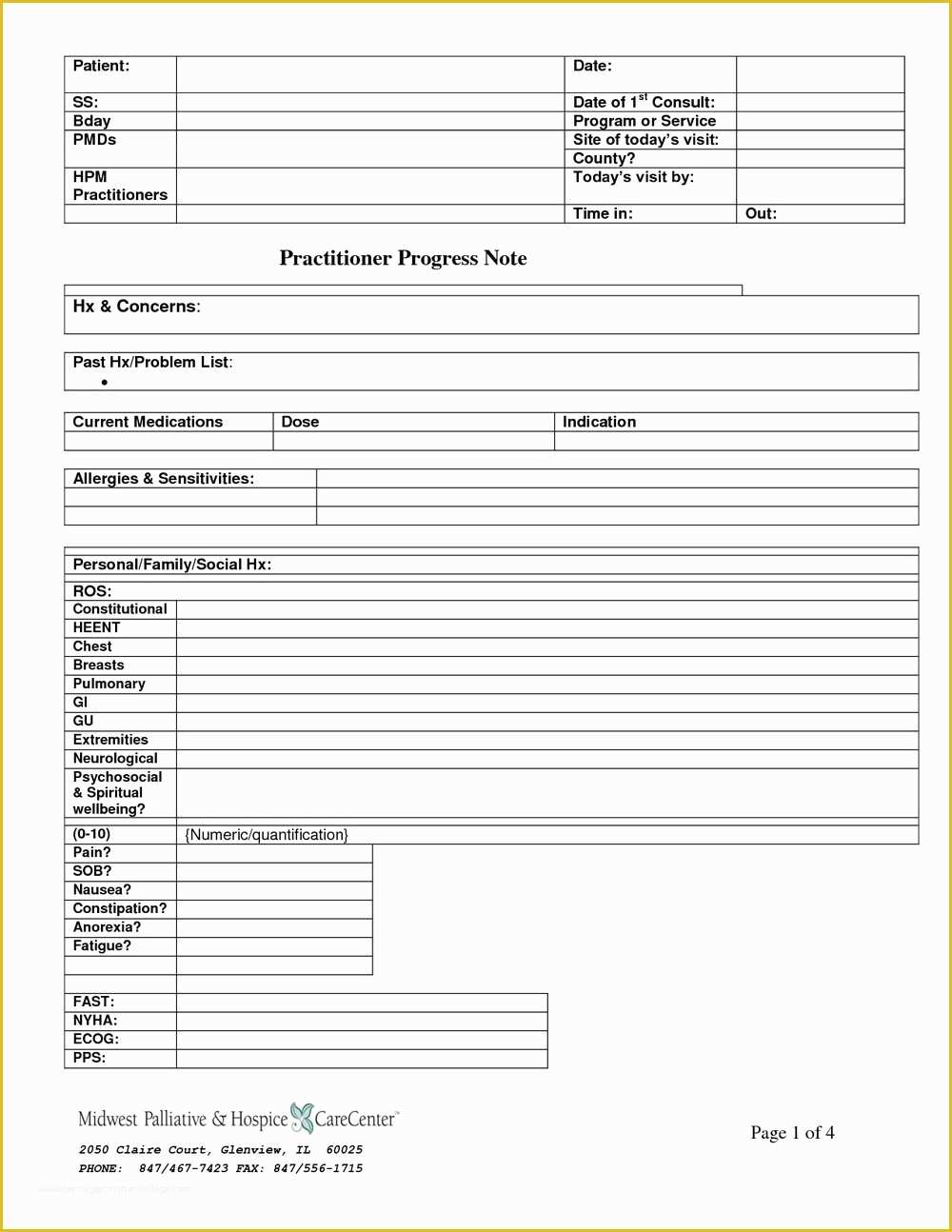
Psychiatric Evaluation form Template Luxury Sample Psychosocial
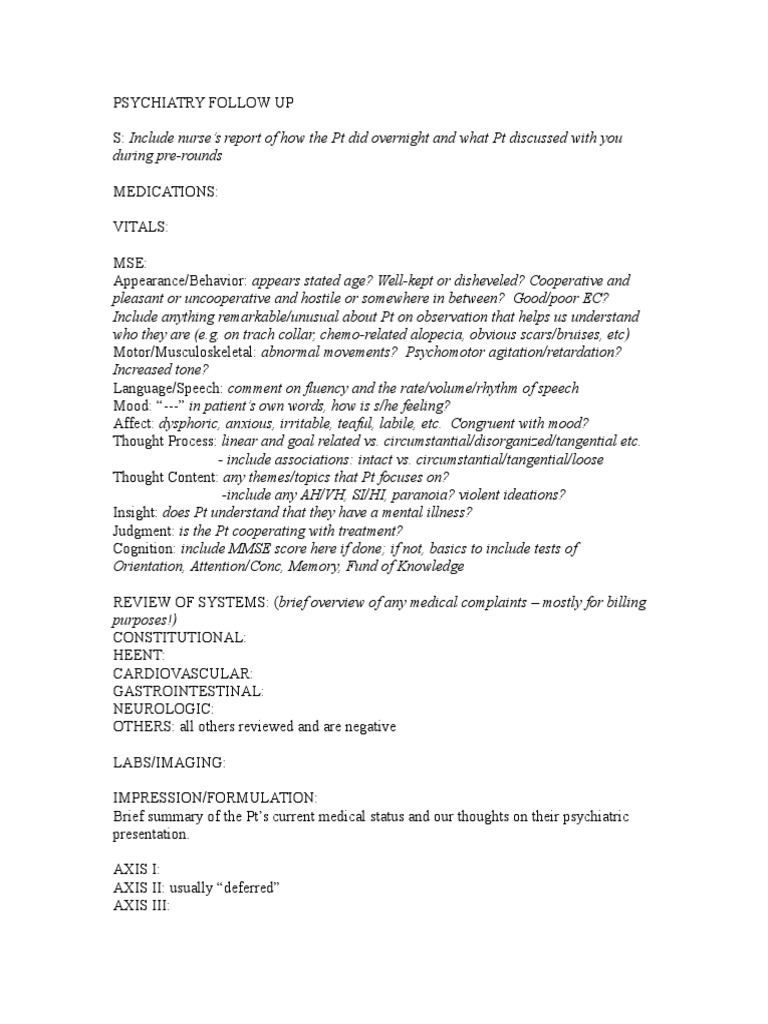
PSYCH Followup Template PDF
Psychiatry Em Note Template
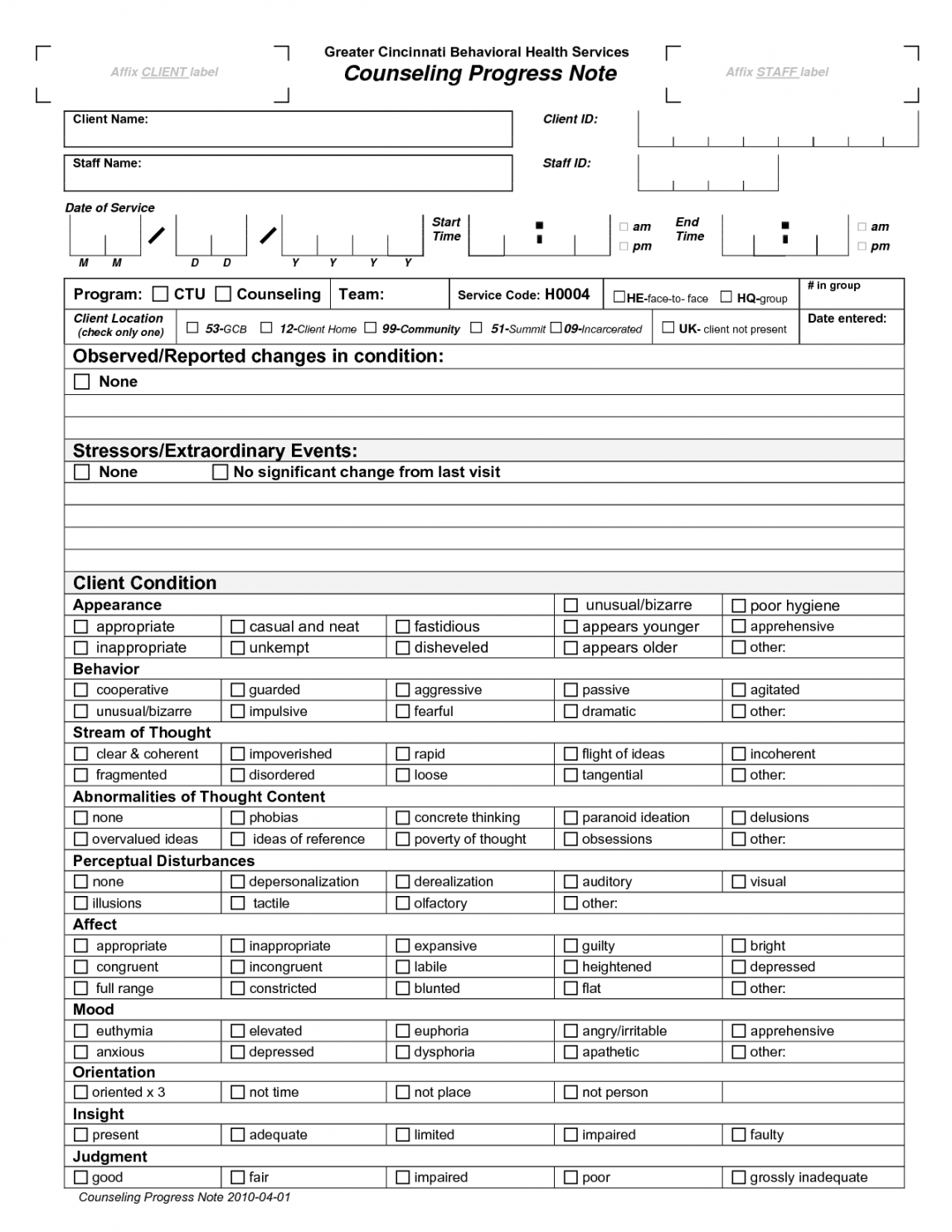
Editable Pin En Terapia Psychiatric Progress Note Template PDF IDTcenter
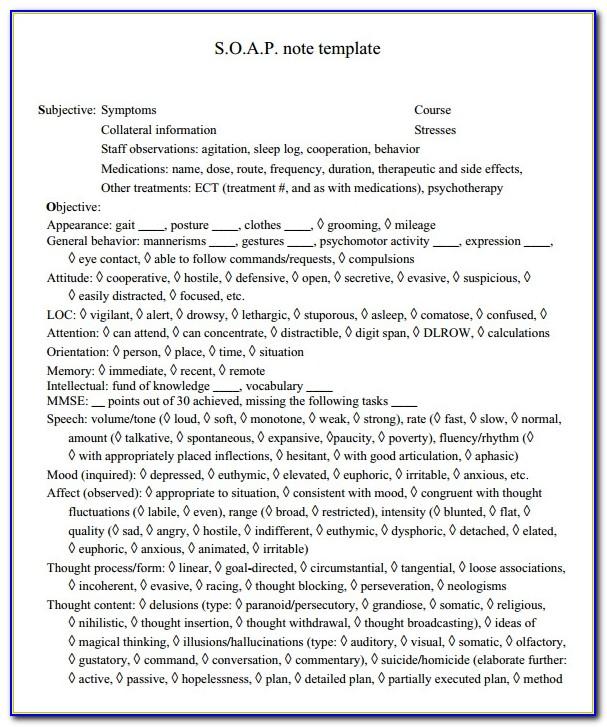
S.o.a.p. Note Template For Psychiatry printable pdf download
editable reading your notes psychiatry follow up note template pdf in
Psychiatric Progress Note Template
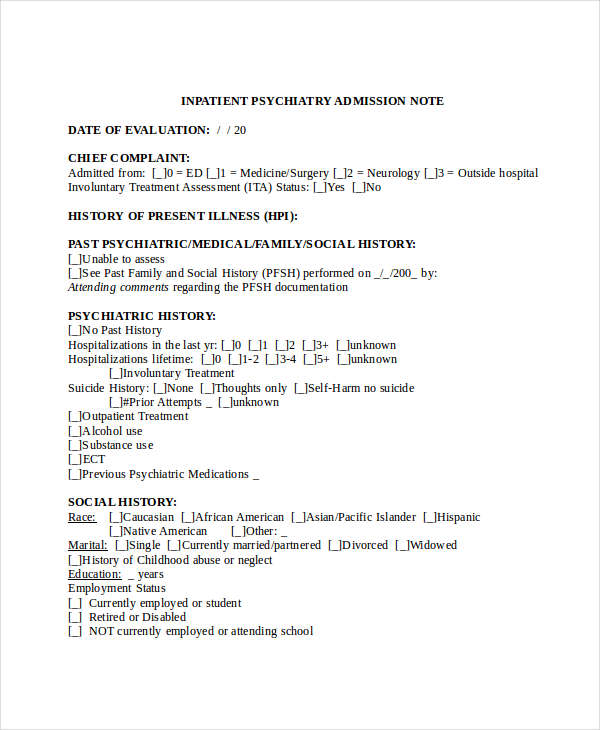
Inpatient Psychiatric Progress Note Sample
Web A Psychiatric Progress Note Is Vital For Tracking Each Of Your Patient’s Progress, As Well As Helping You Run A Successful Psychiatric Practice.
Web This Will Also Give You A Good Understanding Of The Clinical Content Available In Our Notes Templates.
Web [Select Name=Variable_2 Value=In The Past 24 Hours|In The Past 48 Hours|Since Admission], Patient [Select Name=Variable_3 Value=Has|Has Not] Required.
Three Types Of Clinical Psychiatric Evaluations Are Discussed:
Related Post: